Current Issue: Volume 1 | Issue 1 | Year 2025
Institutional Subscription
Individual Subscription
Original Article

Siddharth Manoj, Advait Bhuran, Rashmi Hansdah, Vidhu Sharma, Sarbesh Tiwari, Kapil Soni, Amit Goyal
Abstract
Background: Otosclerosis is a progressive disease causing stapes fixation and conductive hearing loss. While tympanometry and high-resolution computed tomography (HRCT) are commonly used for diagnosis, their accuracy varies. This study evaluates the diagnostic performance of these modalities individually and in combination, using intraoperative findings as the reference standard.
Methods: A retrospective analysis of 40 patients who underwent exploratory tympanotomy for suspected otosclerosis was conducted. Preoperative tympanometry and HRCT findings were compared to intraoperative confirmation. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated. McNemar’s test assessed statistical significance.
Results: Tympanometry had high sensitivity (78.13%) but low specificity (50%), whereas HRCT had lower sensitivity (43.75%) but higher specificity (62.6%). Combining both improved specificity (75%) but reduced sensitivity (37.5%). PPV remained high (85.7% for the combined test), indicating substantial predictive value when both tests were positive. However, NPV was consistently low, limiting their reliability in ruling out otosclerosis. Statistical analysis showed no significant change in diagnostic accuracy when combining tests.
Conclusion: Tympanometry is helpful for screening, while HRCT aids in confirmation. However, neither test, alone nor in combination, reliably excludes otosclerosis due to low NPV. Preoperative HRCT interpretation should involve experienced radiologists, and emerging imaging techniques may enhance diagnostic accuracy.
Keywords: Conductive Hearing Loss, High Resolution Computed Tomography, Otosclerosis, Tympanometry.
Abstract
In this era of microvascular reconstruction, where the practise of microvascular surgery is widely practised by many surgeons, reconstruction with free flap has become mandatory in most of the head and neck oncological procedures. However, due to its difficult learning curve and time-consuming nature, free flaps are not routine surgery for many surgeons. The success of free tissue transfer surgery is not solely determined by the surgeon’s skills alone. Age and operative time can cause medical complications, if not surgical complications, and hence can lead to free flap failure. There are some lesions where local and regional flaps still hold their value as a good substitute for free flaps. The submental flap is one such flap. Though the utility and safety of the submental flap in oncological surgery has been questioned by many, with proper case selection and proper technique, the submental flap is still good and safe in oral cavity reconstruction. The purpose of this paper is to present a series of 13 patients who had undergone reconstruction with submental flaps after resection of their primary tumours in the oral cavity. Key words: Oral cancer, reconstruction, submental flap

Jijitha Lakshmanan, Hanifa Akhtar, N.Brian Shunyu, Ruuzeno Kuotsu, Aswathi K V, Nisha Kumari
Abstract
Material and Methods: Our current study included 213 participants who presented to the ENT Outpatient Department in a tertiary institute in North Eastern India with complaints of giddiness or vertigo during the period from April 2024 to December 2024. Required clinical data was collected by verification of medical records maintained in the vertigo clinic. And etiologic distribution for vertigo was also studied.
Results: Of the 213 patients studied, 62.79% were females, and 37.21% were males. The median age range of the population was 45-60 years.
The etiologies for vertigo prevalent in the study population were: Benign Paroxysmal Positional Vertigo (BPPV) (34.74%) Vestibular Migraine (26.29%), Meniere’s Disease (18.3%), Central vertigo (5.16%), Labyrinthitis (3.38%), Vestibular Neuronitis (2.81%) and a spectrum of other rare etiologies. A few cardiovascular and functional causes of giddiness were also identified.
Conclusion: BPPV involving the posterior semicircular canal is the most common etiology of vertigo in the study population. Vestibular Migraine and Meniere’s Disease respectively represented the second and third common etiologies. A few rare peripheral vestibular, neurological, and cardiovascular causes were also identified.
Keywords:Vertigo, Giddiness, Vertigo clinic, BPPV, Etiology
Case Reports
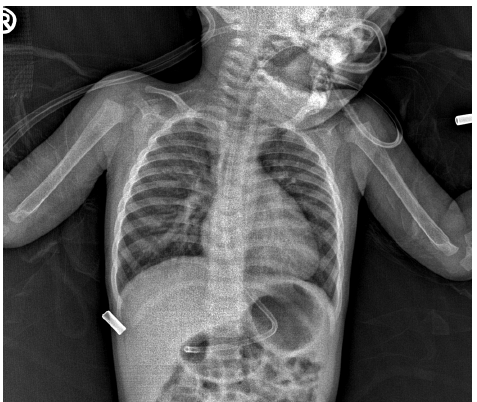
The Wandering Obstruction: A Case of Migratory Foreign Body in the Pediatric Airway
Nithin Prakasan Nair, Joel Alex Sherry, Sivaraman G, Sunitha V C, Mohan VK, Tamil Selvan
Abstract
Introduction: Aspiration of foreign body in the pediatric population is a common yet potentially fatal event, particularly in those under three years of age. Due to their natural tendency to explore objects orally, infants and toddlers are at an increased risk of airway obstruction. This report highlights a case of a migratory foreign body in the airway, emphasizing the diagnostic and management challenges encountered.
Case Report: A 1-year-old male presented with a cough and respiratory distress persisting for three days. Despite initial treatment with antibiotics and oxygen support at an outside hospital, his condition did not improve. Although no clear history of foreign body aspiration was given, further questioning revealed a prior choking episode. Clinical examination suggested left bronchial obstruction, but HRCT thorax unexpectedly showed an isodense right main bronchus foreign body. Intraoperatively, rigid bronchoscopy revealed a large, smooth-surfaced Sitaphal seed lodged in the left main bronchus, indicating migration. Successful removal was achieved despite the retrieval challenges, and the child recovered well postoperatively.
Conclusion: This case underscores the importance of maintaining a high suspicion for foreign body aspiration in children with unexplained respiratory distress. Migratory airway foreign bodies can present with dynamic clinical and radiological findings, necessitating careful preoperative assessment and intraoperative preparedness. However, the gold standard procedure for diagnosis and management of aspirated foreign body is Rigid bronchoscopy.
Keywords: Bronchoscopy, Foreign Body Aspiration, Airway Foreign Body
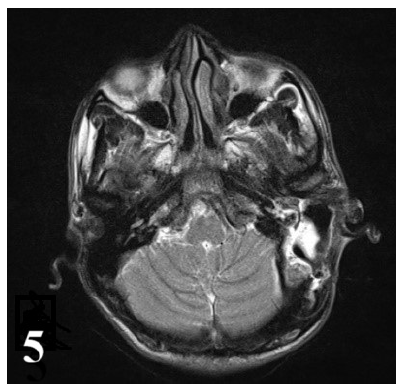
Sauradeep Das, Nayana Sarma, Prachurya Tamuli, Suvamoy Chakraborty
Abstract
Chronic otitis media (COM) is a common ear infection leading to multiple intracranial and extracranial complications. But with the advent of antibiotics, the rate of complications has reduced. Intracranial complications are a dreaded result of such infections, and the rarity of such complications has rendered their treatment a rarity, often reported as isolated case reports. Here we would like to discuss a case of a 20 year old male with cerebellar abscess due to Chronic Otitis Media (COM), along with postauricular abscess and post aural discharge which was treated surgically with mastoid exploration along with concurrent neurosurgical intervention followed by medical management with antibiotic and anticoagulant coverage with complete recovery of the patient. The patient was observed to have a complete recovery with no residual abscess. Three months postoperative follow-up of the patient revealed a healed mastoid cavity with an intact neotympanum. Even though rare and moribund, when treated properly, patients recover completely.
KEYWORDS: otogenic cerebellar abscess, intracranial complication, chronic otitis media, mastoid exploration, multidisciplinary approach.

Ruuzeno Kuotsu, Jijitha Lakshmanan, Hanifa Akhtar
Abstract
Inverted papillomas comprises only 0.4% to 7% among all sinonasal tumors and commonly presents as red, bulky, unilateral, vascular mass and sometimes associated with the presence of polyps. Though benign, it is given special attention because of its increased incidence of recurrence, with a property to cause destruction locally and, in long-standing cases, its association with carcinoma. Its presentation can be very similar to chronic rhinosinusitis with nasal polyposis or an antro-choanal polyp; therefore, it can be misdiagnosed if high clinical suspicion is not kept in mind. Out of the three cases in this series, one case was initially diagnosed as chronic rhinosinusitis with nasal polyposis, a second case was diagnosed as antro-choanal polyp based on clinical, radiological, and pre-operative biopsy reports, and the third case was diagnosed as inverted papilloma
with synchronous squamous cell carcinoma after the preoperative biopsy report. The need to bear in mind the possibility of inverted papilloma, although rare in differential diagnosis of nasal polyposis, is stressed because it necessitates a more complete surgical procedure to avoid recurrence and achieve a better outcome.
Keywords: Inverted papilloma, polyposis, antro-choanal polyp.

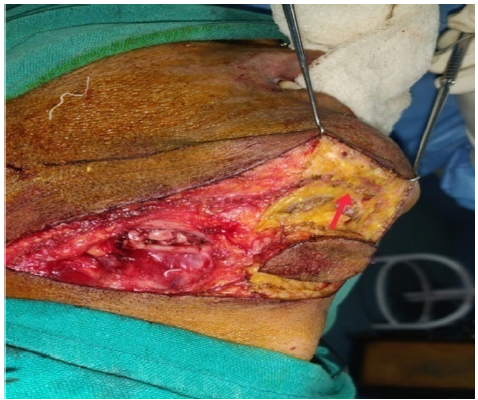
Jijitha Lakshmanan, Bhaswati Mahanta, T Paramesha Patra
Abstract
Introduction: Lipoma arises from adipose cells, which are benign, mesenchymal tumors. They can be present all over the body, and around 13% are located in the head and neck region, but rarely occurs in the anterior aspect of the neck.
Case report: A 25-year-old woman presented with swelling in the anterior part of her neck. The swelling clinically resembled a thyroid swelling. But on evaluation, it turned out to be a lipoma. Surgical excision of the swelling was done.
Conclusion: Lipoma presenting in the anterior part of the neck is rare. It usually mimics a thyroid swelling. Evaluation with imaging and Fine needle aspiration cytology (FNAC) leads to proper diagnosis and helps in appropriate intervention.
Keywords: Lipoma, swelling, neck
Review Article

Hanifa Akhtar, Ruuzeno Kuotsu, Jijitha Lakshmanan